
Back Fibromialgie Afrikaans ألم عضلي ليفي Arabic Fibromialxa AST Fibromialgiya Azerbaijani فیبرومیالژی AZB Фибромиалгия Bulgarian ফাইব্রোমায়ালজিয়া Bengali/Bangla Fibromiàlgia Catalan فایبرۆمایێلجا CKB Fibromyalgie Czech
| Fibromyalgia | |
|---|---|
| Other names | Fibromyalgia syndrome |
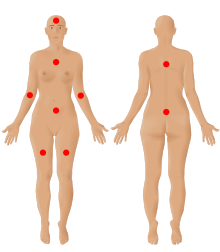 | |
| The nine possible pain sites of fibromyalgia according to the American Pain Society. | |
| Pronunciation | |
| Specialty | Rheumatology, neurology[2] |
| Symptoms | Widespread pain, feeling tired, sleep problems[3][4] |
| Usual onset | Early-Middle age[5] |
| Duration | Long term[3] |
| Causes | Unknown[4][5] |
| Diagnostic method | Based on symptoms after ruling out other potential causes[4][5] |
| Differential diagnosis | Anemia, autoimmune disorders (such as ankylosing spondylitis, polymyalgia rheumatica, rheumatoid arthritis, scleroderma, or multiple sclerosis), Lyme disease, osteoarthritis, thyroid disease[6][7] |
| Treatment | Sufficient sleep and exercise[5] |
| Medication | Duloxetine, milnacipran, pregabalin, gabapentin[5][8] |
| Prognosis | Normal life expectancy[5] |
| Frequency | 2%[4] |
Fibromyalgia is a medical syndrome that causes chronic widespread pain, accompanied by fatigue, awakening unrefreshed, and cognitive symptoms. Other symptoms can include headaches, lower abdominal pain or cramps, and depression.[9] People with fibromyalgia can also experience insomnia[10] and general hypersensitivity.[11][12] The cause of fibromyalgia is unknown, but is believed to involve a combination of genetic and environmental factors.[4] Environmental factors may include psychological stress, trauma, and some infections.[4] Since the pain appears to result from processes in the central nervous system, the condition is referred to as a "central sensitization syndrome".[4][13] Although a protocol using an algometer (algesiometer) for determining central sensitization has been proposed as an objective diagnostic test, fibromyalgia continues to be primarily diagnosed by exclusion despite the high possibility of misdiagnosis.[14]
Fibromyalgia was first defined in 1990, with updated criteria in 2011,[4] 2016,[9] and 2019.[12] The term 'fibromyalgia' is from Neo-Latin fibro-, meaning 'fibrous tissues'; Greek μυο- myo-, 'muscle'; and Greek άλγος algos, 'pain'; thus, the term literally means "'muscle and fibrous connective tissue pain'.[15] Fibromyalgia is estimated to affect 2 to 4% of the population.[16] Women are affected about twice as often as men.[4][16] Rates appear similar across areas of the world and among varied cultures.[4]
The treatment of fibromyalgia is symptomatic[17] and multidisciplinary.[18] The European Alliance of Associations for Rheumatology strongly recommends aerobic and strengthening exercise.[18] Weak recommendations are given for mindfulness, psychotherapy, acupuncture, hydrotherapy, and meditative exercise such as qigong, yoga, and tai chi.[18] The use of medication in the treatment of fibromyalgia is debated,[18][19] although antidepressants can improve quality of life.[20] Other medications commonly considered helpful in managing fibromyalgia include serotonin–norepinephrine reuptake inhibitors, nonsteroidal anti-inflammatory drugs, and muscle relaxants.[21] Q10 coenzyme and vitamin D supplements may reduce pain and improve quality of life.[22] While symptoms of fibromyalgia are persistent in nearly all patients, they are not caused by cell damage or any organic disease.[19]
- ^ "fibromyalgia". Collins Dictionaries. Archived from the original on 4 October 2015. Retrieved 16 March 2016.
- ^ "Neurology Now: Fibromyalgia: Is Fibromyalgia Real? | American Academy of Neurology". tools.aan.com. October 2009. Retrieved 1 June 2018.[permanent dead link]
- ^ a b Cite error: The named reference
pmid21303476was invoked but never defined (see the help page). - ^ a b c d e f g h i j Clauw DJ (April 2014). "Fibromyalgia: a clinical review". JAMA. 311 (15): 1547–1555. doi:10.1001/jama.2014.3266. PMID 24737367. S2CID 43693607.
- ^ a b c d e f Cite error: The named reference
NIH2014Txwas invoked but never defined (see the help page). - ^ Ferri FF (2010). "Chapter F". Ferri's differential diagnosis: a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders (2nd ed.). Philadelphia, PA: Elsevier/Mosby. ISBN 978-0-323-07699-9.
- ^ Schneider MJ, Brady DM, Perle SM (2006). "Commentary: differential diagnosis of fibromyalgia syndrome: proposal of a model and algorithm for patients presenting with the primary symptom of chronic widespread pain". Journal of Manipulative and Physiological Therapeutics. 29 (6): 493–501. doi:10.1016/j.jmpt.2006.06.010. PMID 16904498.
- ^ Cite error: The named reference
Coch2017Gabwas invoked but never defined (see the help page). - ^ a b Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Häuser W, Katz RL, et al. (December 2016). "2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria". Seminars in Arthritis and Rheumatism. 46 (3): 319–329. doi:10.1016/j.semarthrit.2016.08.012. PMID 27916278.
- ^ Cite error: The named reference
Wu-2017was invoked but never defined (see the help page). - ^ Cite error: The named reference
Hauser2019was invoked but never defined (see the help page). - ^ a b Cite error: The named reference
Arnold-2019was invoked but never defined (see the help page). - ^ Cite error: The named reference
Central sensitivity and fibromyalgiwas invoked but never defined (see the help page). - ^ Cite error: The named reference
:6was invoked but never defined (see the help page). - ^ Bergmann U (2012). Neurobiological foundations for EMDR practice. New York: Springer Pub. Co. p. 165. ISBN 978-0-8261-0938-5.
- ^ a b Fitzcharles MA, Cohen SP, Clauw DJ, Littlejohn G, Usui C, Häuser W (May 2021). "Nociplastic pain: towards an understanding of prevalent pain conditions". Lancet. 397 (10289): 2098–2110. doi:10.1016/s0140-6736(21)00392-5. PMID 34062144. S2CID 235245552.
- ^ Cite error: The named reference
Prab2019was invoked but never defined (see the help page). - ^ a b c d Cite error: The named reference
Macfarlane-2017was invoked but never defined (see the help page). - ^ a b Cite error: The named reference
Hauser2018was invoked but never defined (see the help page). - ^ Cite error: The named reference
Mascarenhas-2021was invoked but never defined (see the help page). - ^ Kia S, Choy E (May 2017). "Update on Treatment Guideline in Fibromyalgia Syndrome with Focus on Pharmacology". Biomedicines. 5 (2): 20. doi:10.3390/biomedicines5020020. PMC 5489806. PMID 28536363.
- ^ Cite error: The named reference
Ibáñez-Vera-2018was invoked but never defined (see the help page).