Melatonin is a naturally occurring hormone produced in the brain that is also used as a dietary supplement and medication.[9][12] As a hormone, melatonin is released by the pineal gland and is involved in sleep–wake cycles.[9][12] As a supplement, it is often used for the attempted short-term treatment of disrupted sleep patterns, such as from jet lag or shift work, and is typically taken orally.[13][14][15] There is evidence of its benefit for this use, but is not strong.[16] A 2017 review found that sleep onset occurred six minutes faster with use on average, but found no change in total time asleep.[14]
Side effects from melatonin supplements are minimal at low doses for short durations (the studies reported about equally for both melatonin and placebo).[9][17] Side effects of melatonin are rare but may occur in 1 to 10 patients in 1,000.[17][8] They may include somnolence, headaches, nausea, diarrhea, abnormal dreams, irritability, restlessness, insomnia, anxiety, migraine, lethargy, hyperactivity, dizziness, hypertension, abdominal pain, heartburn, mouth ulcers, dry mouth, hyperbilirubinaemia, dermatitis, night sweats, pruritus, rash, dry skin, pain in the extremities, symptoms of menopause, chest pain, glycosuria (sugar in the urine), proteinuria (protein in the urine), abnormal liver function tests, weight gain, mood swings, aggression, and grogginess after awakening.[8][18][17][19][20] Its use is not recommended during pregnancy or breastfeeding or for those with liver disease.[15][20]
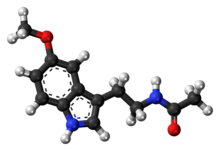
Melatonin acts as an agonist of the melatonin MT1 and MT2 receptors, the biological targets of endogenous melatonin.[21] It is thought to activate these receptors in the suprachiasmatic nucleus of the hypothalamus in the brain to regulate the circadian clock and sleep–wake cycles.[21] Immediate-release melatonin has a short elimination half-life of about 20 to 50 minutes.[22][9][10] Prolonged-release melatonin used as a medication has a half-life of 3.5 to 4 hours.[11][8]
Melatonin was discovered in 1958.[9] It is sold over-the-counter in Canada and the United States;[17][19] in the United Kingdom, it is a prescription-only medication.[15] In Australia and the European Union, it is indicated for difficulty sleeping in people over the age of 54.[23][8] In the European Union, it is indicated for the treatment of insomnia in children and adolescents.[18] The U.S. Food and Drug Administration (FDA) treats melatonin as a dietary supplement and, as such, has not approved it for any medical uses.[17] It was approved for medical use in the European Union in 2007.[8] Besides melatonin, certain synthetic melatonin receptor agonists like ramelteon, tasimelteon, and agomelatine are also used in medicine.[24][25] In 2022, it was the 217th most commonly prescribed medication in the United States, with more than 1 million prescriptions.[26][27]
- ^ "Melatonin – Drugs.com". Drugs.com. Retrieved 12 October 2018.
- ^ "Melatonin". Sleepdex. Retrieved 17 August 2011.
- ^ a b https://www.tga.gov.au/resources/auspar/auspar-melatonin-1 [bare URL]
- ^ a b c "Pros and cons of melatonin". Mayo Clinic. Retrieved 20 August 2022.
- ^ https://www.tga.gov.au/resources/auspar/auspar-melatonin-link-immela-melakso-voquily [bare URL]
- ^ Cite error: The named reference
TordjmanSwas invoked but never defined (see the help page). - ^ a b Cite error: The named reference
pmid33540815was invoked but never defined (see the help page). - ^ a b c d e f g h Cite error: The named reference
Circadin-Labelwas invoked but never defined (see the help page). - ^ a b c d e f Auld F, Maschauer EL, Morrison I, Skene DJ, Riha RL (August 2017). "Evidence for the efficacy of melatonin in the treatment of primary adult sleep disorders" (PDF). Sleep Medicine Reviews. 34: 10–22. doi:10.1016/j.smrv.2016.06.005. hdl:20.500.11820/0e890bda-4b1d-4786-a907-a03b1580fd07. PMID 28648359.
- ^ a b Hardeland R, Poeggeler B, Srinivasan V, Trakht I, Pandi-Perumal SR, Cardinali DP (2008). "Melatonergic drugs in clinical practice". Arzneimittelforschung. 58 (1): 1–10. doi:10.1055/s-0031-1296459. PMID 18368944. S2CID 38857779.
- ^ a b Cite error: The named reference
pmid23044640was invoked but never defined (see the help page). - ^ a b Faraone SV (2014). ADHD: Non-Pharmacologic Interventions, An Issue of Child and Adolescent Psychiatric Clinics of North America, E-Book. Elsevier Health Sciences. p. 888. ISBN 978-0-323-32602-5.
- ^ Buscemi N, Vandermeer B, Pandya R, Hooton N, Tjosvold L, Hartling L, et al. (November 2004). "Melatonin for treatment of sleep disorders" (PDF). Evidence Report/Technology Assessment No. 108. (Prepared by the University of Alberta Evidence-based Practice Center, Under Contract No. 290-02-0023.) AHRQ Publication No. 05-E002-2. Rockville, MD: Agency for Healthcare Research and Quality (108). Agency for Healthcare Research and Quality (AHRQ), US Department of Health and Human Services: 1–7. doi:10.1037/e439412005-001. PMC 4781368. PMID 15635761. Retrieved 5 June 2013.
- ^ a b Matheson E, Hainer BL (July 2017). "Insomnia: Pharmacologic Therapy". American Family Physician. 96 (1): 29–35. PMID 28671376.
- ^ a b c British national formulary: BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 482–483. ISBN 978-0-85711-338-2.
- ^ Brasure M, MacDonald R, Fuchs E, Olson CM, Carlyle M, Diem S, et al. (2015). "Management of Insomnia Disorder[Internet]". AHRQ Comparative Effectiveness Reviews. 15 (16): EHC027–EF. PMID 26844312.
Evidence for benzodiazepine hypnotics, melatonin agonists in the general adult population, and most pharmacologic interventions in older adults was generally insufficient
- ^ a b c d e "Melatonin: Side Effects, Uses, Dosage (Kids/Adults)". Drugs.com. Retrieved 9 January 2019.
- ^ a b "Slenyto EPAR". European Medicines Agency (EMA). 17 September 2018. Retrieved 31 May 2020. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized, provided the source is acknowledged.
- ^ a b "Summary Safety Review – MELATONIN (N-acetyl-5-methoxytryptamine) – Review of the Safety of Melatonin in Children and Adolescents". Government of Canada. Health Canada. 10 December 2015. Retrieved 9 January 2019.
- ^ a b "Melatonin- Oral". Government of Canada. Health Canada. 28 August 2018. Archived from the original on 1 April 2019. Retrieved 9 January 2019.
- ^ a b Pevet P, Challet E, Felder-Schmittbuhl MP (2021). "Melatonin and the circadian system: Keys for health with a focus on sleep". The Human Hypothalamus: Anterior Region. Handbook of Clinical Neurology. Vol. 179. pp. 331–343. doi:10.1016/B978-0-12-819975-6.00021-2. ISBN 9780128199756. PMID 34225973. S2CID 235744969.
- ^ Cite error: The named reference
drugbankwas invoked but never defined (see the help page). - ^ "Australian Public Assessment Report for Melatonin" (PDF). Australian Government Department of Health and Ageing Therapeutic Goods Administration. January 2011. pp. 2, 4. Retrieved 9 January 2019.
Monotherapy for the short term treatment of primary insomnia characterised by poor quality of sleep in patients who are aged 55 or over.
- ^ Williams WP, McLin DE, Dressman MA, Neubauer DN (September 2016). "Comparative Review of Approved Melatonin Agonists for the Treatment of Circadian Rhythm Sleep-Wake Disorders". Pharmacotherapy. 36 (9): 1028–41. doi:10.1002/phar.1822. PMC 5108473. PMID 27500861.
- ^ Atkin T, Comai S, Gobbi G (April 2018). "Drugs for Insomnia beyond Benzodiazepines: Pharmacology, Clinical Applications, and Discovery". Pharmacol Rev. 70 (2): 197–245. doi:10.1124/pr.117.014381. PMID 29487083. S2CID 3578916.
- ^ "The Top 300 of 2022". ClinCalc. Archived from the original on 30 August 2024. Retrieved 30 August 2024.
- ^ "Melatonin Drug Usage Statistics, United States, 2013 - 2022". ClinCalc. Retrieved 30 August 2024.